Don’t let anyone, including doctors, tell you that you will never have children just because you have PCOS. That is simply untrue. While it may take longer for some women with PCOS to get pregnant, it doesn’t mean you can’t. PCOS is a complex metabolic syndrome that affects everyone differently.
If you want to have children but feel worried about your chances, know that you have several things that can help. Don’t lose hope! Let’s learn about the science behind PCOS and pregnancy.
Is It Possible to Get Pregnant With PCOS?
Despite what everyone says, you can get pregnant if you have PCOS. However, many factors play into how easy that will be. As pregnancy requires two people and a host of other perfectly timed factors, some find it takes longer than they wish to get pregnant.
But just because you received a PCOS diagnosis doesn’t mean you can never have kids. You certainly can as long as the right variables line up. So let’s look at some of the considerations that play into PCOS and pregnancy.
Why Is It Hard to Get Pregnant With PCOS?
Some identifying factors of PCOS include undeveloped follicles where eggs develop and missing or irregular periods. So a lack of regular ovulation is the main contributing factor to why some find it difficult to get pregnant.
Imbalances in your hormones can lead to anovulation or poor egg quality. But not every woman with PCOS will experience this as the condition affects everyone differently. Furthermore, male fertility issues can also compound the problem and make it difficult to distinguish what needs treatment.
In addition to ovulation issues, your weight can also affect reproductive health. Fat cells can produce excess estrogen and impact your hormonal balance. And being overweight and having PCOS contributes to insulin resistance and other health risks.
All these factors can reduce your fertility rates and impact ovulation. If you don’t ovulate, there is no egg for the sperm to fertilize.
While many factors may contribute to the difficulty of conceiving, you can get treatment. With the right plan and support, you can make changes to improve your reproductive health and increase your chance of getting pregnant.
How Can I Improve My Fertility With PCOS?
You can improve your fertility in several ways, and combining several methods may have better results. So let’s look at lifestyle modifications and pharmaceutical treatments to improve your chances of getting pregnant with PCOS.
Diet
Eating a healthy diet is essential for overall health and reproductive health. Studies show that eating a high-fiber and high-protein diet with moderate carb intake can help improve insulin resistance, weight, depression, and fertility.
They also show that a low-glycemic index diet and eating small portions in frequent intervals can lead to optimal results.
Not getting enough nutrients and vitamins from your diet can impact your hormonal health and affect your fertility.
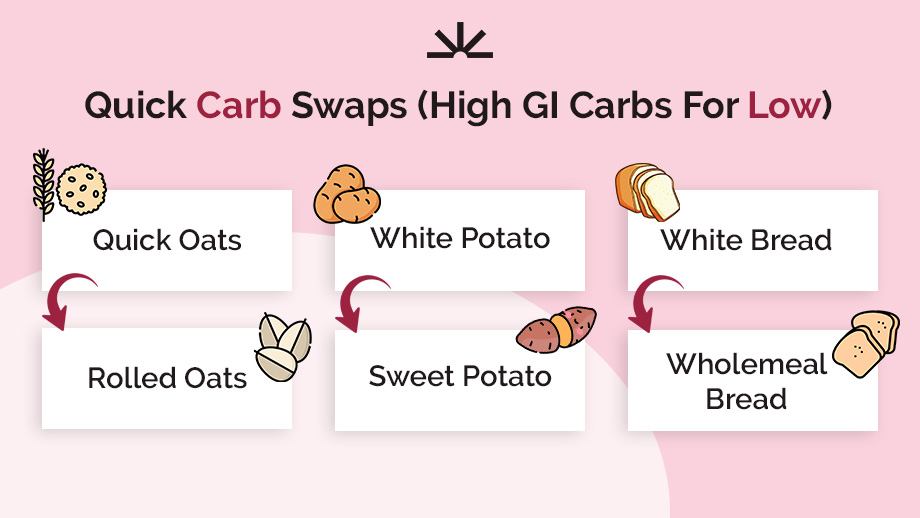
Drew’s Quick Carb Swaps For PCOS
Exercise
Exercise can help improve so many functions of your body. But specifically for PCOS, weight training and resistance exercises combined with moderate-intensity exercise can have great results.
Going on daily walks, staying active, and having a few scheduled workouts in your week will help you lose weight. It can also help improve your ovulation and menstrual regularity, improving fertility outcomes.
But know that any type of physical activity is better than none. Finding one that you enjoy and can be consistent with is key.
And a study showed that combining exercise with other lifestyle changes leads to a “decrease in testosterone, reduced body weight, abdominal fat, body hair growth, and insulin resistance.” All of these can improve reproductive health, stress, and self-image.
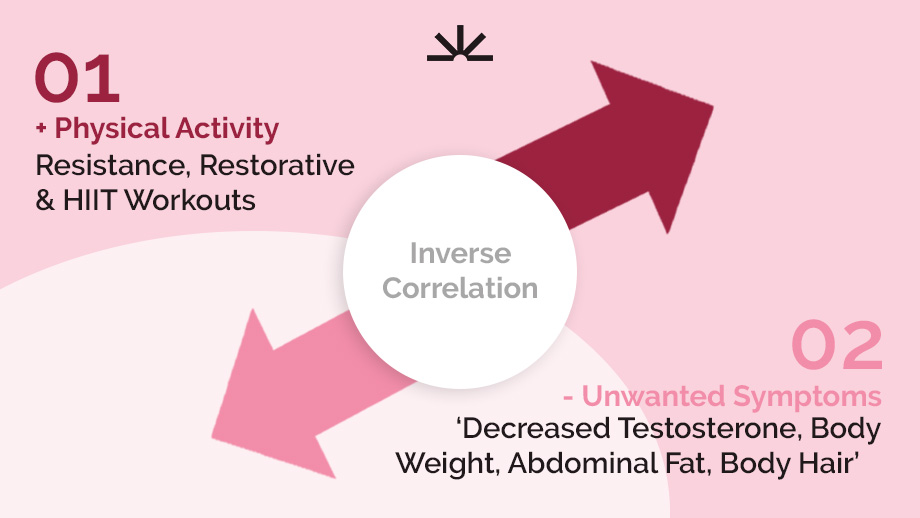
Exercise and Unwanted Symptoms That Can Lead to Poor Reproductive Health Are Inversely Correlated
Stress-Reduction
Reducing outside stressors can help you balance cortisol levels and other hormones in your body. It can also help increase your motivation to exercise, eat well, and care for yourself.
You can lower stress through good sleep routines, meditation, journaling, going outside, and having support.
While you can’t eliminate all your stress, you can find ways to manage it. This can lead to a better mindset and internal landscape for conceiving.
Pro-Ovulation Drugs
Getting pregnant with PCOS may require medical intervention. You can take certain medications to help induce ovulation regularity and quality. These can work well for people who have a hard time conceiving.
You can talk to your doctor about your options. Some prescription medications, like Clomid and Letrozole, have good success rates. Keep reading to learn more about these.
Supplements
Taking supplements to support your reproductive health can have great outcomes. The right supplementation can help balance hormones, promote ovulation, and decrease pregnancy risks. Let’s learn more about which supplements work for women with PCOS and fertility.
What Supplements Should I Take to Improve Fertility With PCOS?
Prenatal vitamins help prevent complications and certain congenital disorders. Taking these supplements before conceiving and during pregnancy can lead to a healthier pregnancy. And some can even help improve your chances of getting pregnant with PCOS.
NAC
N-Acetylcysteine (NAC), an antioxidant and amino acid, helps to improve insulin resistance. However, a review and meta-analysis of eight studies showed, “Women with NAC had higher odds of having a live birth, getting pregnant, and ovulation as compared to placebo.” Taking this supplement can improve outcomes for women with PCOS who want to get pregnant.
Myo Inositol
Studies show that Myo-inositol can work as a great fertility treatment option for women with PCOS. It can help improve insulin sensitivity, egg quality, and fertilization, ovulation, and pregnancy rates, and IVF treatment.
Another exciting result said, “The achieved pregnancy rates are at least in an equivalent or even superior range than those reported using metformin as an insulin sensitizer. No moderate to severe side effects were observed when Myo-inositol was used at a dosage of 4000 mg per day.”
So, in addition to the many fertility benefits of Myo-inositol, it also comes with fewer side effects and can even work better than metformin. This can be a game changer for women who can’t tolerate other prescription options.

Charlotte F / H&B Vitamins Customer
Vitamin D
Vitamin D is an essential hormone we can’t live without. You can get it from food and sunlight. Women with PCOS, however, have higher rates of vitamin D deficiency which can cause pregnancy-related complications and health risks.
But with optimal levels, it can improve fertility and decrease pregnancy complications. You can chat with your doctor about the best way to obtain and maintain your vitamin D levels to help you conceive.
What Fertility Medication Can Help Me Get Pregnant?
To get pregnant, your body first needs to release a healthy egg. This means you need to ovulate. Thus, you can improve your fertility with PCOS by inducing regular ovulation. Some medications can help this process. Let’s look at a few most common ones.
Letrozole Versus Clomid
Letrozole and clomiphene, commonly known as Clomid, induce ovulation and help you do so more regularly. Like you know, getting pregnant with PCOS can be difficult if you don’t ovulate.
These medications work to block the conversion of androgens to estrogens. It also stimulates the brain to produce follicle-stimulating hormone (FSH), which leads to follicles releasing a mature egg.
In studies, letrozole has had a higher ovulation rate of 68.7% versus 48.3% with Clomid. And Letrozole also has higher live birth rates at 27.5% versus Clomid at 19%.
However, researchers found that taking Letrozole and Clomid together had an ovulation rate of 73%.
But know that these medications come with side effects. When taking Clomid, women may experience hot flashes, breast tenderness, stomach pain, nausea, vomiting, headaches, and spotting.
Side effects of letrozole include headaches, dizziness, hot flashes, fatigue, joint pain, and flushing. Even when you stop taking it, you may experience some residual side effects as it takes time for it to leave the body.
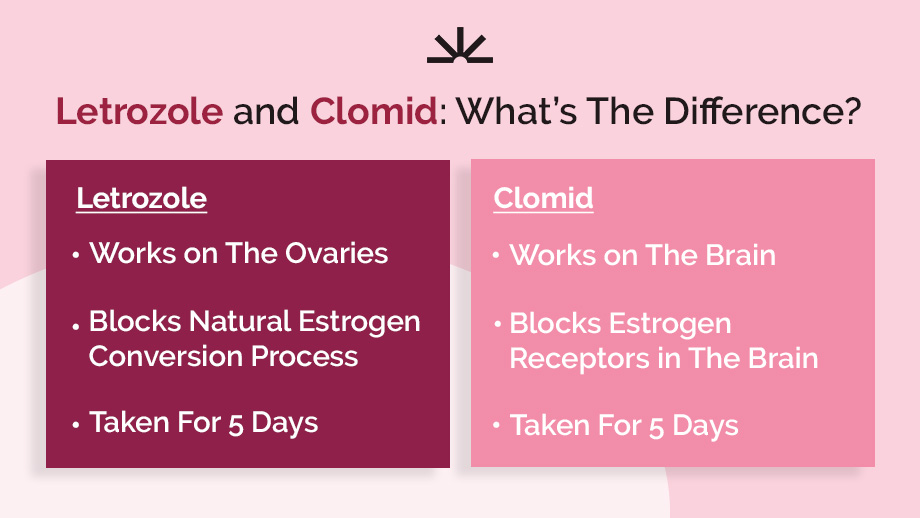
Letrozole and Clomid: What’s The Difference?
Metformin
Metformin, a common diabetes medication, works to sensitize the body to insulin and manage blood sugar levels. Doctors often prescribe it for women with PCOS who also have insulin resistance. But in addition to improving this important hormone response in the body, it can also help induce ovulation.
In an article from the National Library of Medicine, metformin can induce ovulation through actions “such as reducing insulin levels and altering the effect of insulin on ovarian androgen biosynthesis, theca cell proliferation, and endometrial growth.”
This means it can improve the endometrial lining, which forms a nice cozy home for the embryo. They also found that it can reduce the production of androgens in the ovaries. With lower androgens, your ovaries can release a healthy egg.
The study also showed Clomid and metformin had the same effectiveness rate. But the combination of the two, versus Clomid alone, resulted in higher pregnancy and ovulation.
Some side effects of metformin include nausea, vomiting, upset stomach, diarrhea, and vitamin B12 deficiency. This deficiency can also cause other serious side effects.
Does FSH:LH Ratio Increase the Chances of Ovulation?
Luteinizing hormone (LH) and follicle-stimulating hormone (FSH) come from the pituitary gland in the brain. These hormones stimulate follicle growth and ovulation.
Right before you ovulate, your body will produce a surge of these hormones to stimulate ovulatory functions and release an egg. However, if these ratios are out of balance, either too high or too low, it can affect your ability to ovulate.
According to a study with 1,000 women, “Elevated LH/FSH ratio appears to have adverse effects on the number of follicles and oocytes, as well as on follicles quality, oocyte maturation and granulosa cell function.”
This means that your follicles which grow to release an egg, do not fully mature. And high LH can lead to an early response throwing off the ovulation cycle.
If you don’t produce mature eggs at the right time in your cycle, it will limit your chances of getting pregnant. You can ask your doctor to test these levels to see if they are too high or too low.
Based on the study, elevated LH/FSH ratios were associated with lower ovulation but better pregnancy and live birth rates. The issue is that the right ratio depends on where you are in your cycle.
Do I Need to See a Fertility Specialist if I Have PCOS?
Deciding to see a fertility specialist is a personal decision you can make with your partner and doctor.
Most physicians recommend a fertility specialist for women under 35 with PCOS if they have tried getting pregnant for one year without success. If you are over 35, then you can go after six months of unprotected sex.
Additionally, if you have missing periods or go several months between them and suspect you don’t ovulate regularly, you may choose to see a fertility specialist. However, some doctors may refer a woman with PCOS to a reproductive endocrinologist for other reasons as well.

Fertility Specialist Appointment / New Africa
Are There Any Pregnancy Risks Associated With PCOS?
There are many inherent risks associated with any pregnancy. However, with PCOS, these risks are elevated. Some of the most common include gestational diabetes, preeclampsia, high blood pressure, miscarriage, and preterm birth.
Gestational Diabetes and PCOS
Gestational diabetes impacts the cell’s reception of energy through sugar. According to a study, this can complicate 40% to 50% of PCOS pregnancies. “GDM has been shown to complicate PCOS pregnancy more frequently than normal pregnancy in majority of studies.”
Luckily, you can effectively manage this through diet, exercise, medication, and monitoring. It also often resolves after birth. However, it can pose certain risks for the baby and mother, including jaundice, breathing problems, and high blood pressure.
High Blood Pressure
High blood pressure, or hypertension, in pregnancy can lead to stroke, kidney and heart disease, and fetal complications. Monitoring your blood pressure before and during pregnancy is very important.
“Two large meta-analyses found a two- to four-fold increased rate of pregnancy-induced hypertension (PIH) as well as preeclampsia in women with PCOS,” according to a study.
But you can manage this with blood pressure medication, aspirin, and a healthy diet and exercise plan. You’ll also need to keep up with your regular prenatal visits to monitor your and your baby’s health. High blood pressure can lead to worse conditions, such as preeclampsia.
Preeclampsia
Preeclampsia is a dangerous and sometimes fatal pregnancy risk due to a sudden increase in blood pressure. This can affect vital organs such as the liver, kidney, and brain.
It can also lead to eclampsia which can cause seizures, organ damage, and sometimes death. The only way to currently resolve preeclampsia is delivery. But with the right monitoring, this can be overcome, sometimes with preterm or cesarean birth.
Scientists still don’t know why PCOS causes a higher risk of developing preeclampsia. Additionally, some studies have not found much of an increased risk due to PCOS but rather due to BMI. But more research is needed.
Miscarriage and PCOS
According to a study on miscarriage rates with PCOS, “[Early pregnancy loss] occurs in 30 to 50% of PCOS women compared with 10 to 15% of normal women.”
Researchers believe a probable cause of miscarriage in PCOS is due to hyperandrogenemia — or too much male sex hormones in the body.
Androgen levels can negatively affect estrogen’s role during implantation and endometrial development. Thus, some scientists believe this can lead to early pregnancy loss. However, we need more research on this.
And while the statistics may feel scary, remember that the risks affect all women, and many factors contribute to these numbers. Additionally, with proper prenatal care, you can lower these risks significantly.
Preterm Birth
Due to many factors, such as high blood pressure, gestational diabetes, and others, women with PCOS have a higher risk of preterm birth — mainly because these conditions usually necessitate an early delivery or c-section.
One study says, “For the 908 PCOS women with singleton pregnancy, the mean gestational age at delivery was 38.7 weeks, and preterm delivery occurred in 12.9% of pregnancies.”
Women without PCOS had a preterm delivery rate of 7.4%. While this is a significant increase, the rate is still low. Among the 908 women in the study, the average pregnancy length was 38.7 weeks. Doctors consider 39 to 40 weeks gestational age full term.

Pregnancy Risks Associated With PCOS
How Can I Maintain a Healthy Pregnancy With PCOS?
If you want to have children, you can start preparing early for a healthy pregnancy with PCOS. The proper diet, exercise, and supplementation plan can go a long way to ensure good outcomes.
Additionally, reducing stress and having a positive outlook can also help significantly. As we know, stress can affect your mind and your hormones.
Finally, early and regular monitoring before and during pregnancy can reduce your risk of complications and catch issues early on.
Don’t be afraid to go to the doctor with any concerns, and make plans for your and your baby’s health. If you feel something is off, seek attention immediately, even if it is nothing.
Just because you have PCOS doesn’t mean you can never have children or have to fear dangerous complications. Pregnancy has many risks, no matter the woman.
Understanding how PCOS and your body work can help you take steps to improve your health and get pregnant. You also have many options available to help you conceive.
Is getting pregnant with PCOS hard for you? Share your experiences below.



One Response
Appreciating the time and effort you put into your blog
and in depth information yoou provide. It’s good to come
acrss a blog every once in a while that isn’t the same outdated rehashed information.
Wonderful read! I’ve bookmarked your site and I’m adding your
RSS feeds to my Google account.